- What Is Breast Reconstruction?
- Our Approach on Breast Reconstruction
- Breast Reconstruction Candidates
- Preparing for Breast Reconstruction
- Immediate vs. Delayed Breast Reconstruction
- Breast Reconstruction Options After Mastectomy
- Types of Flap Reconstruction
- Breast Reconstruction Timeline
- Single- vs. Two-Stage Breast Reconstruction
- Breast Reconstruction Follow-Up Appointments
- Nipple & Areola Reconstruction
- Breast Reconstruction Risks
- Breast Reconstruction Recovery
- Breast Reconstruction Insurance Coverage
- Additional Breast Reconstruction FAQs
What Is Breast Reconstruction?
Breast reconstruction surgery is intended to recreate the natural form of the breast after tissue was removed due to cancer or disease. This may involve using breast implants or your own tissue to restore the size and shape of the breasts, and can often be performed at the time of a mastectomy (or other treatment) or later in a delayed procedure. Our board-certified plastic surgeon, Dr. Neil J. Zemmel, is highly experienced in performing a variety of breast reconstruction techniques, and he takes great pride in helping women on their journey to feeling like themselves again.
Our Approach on Breast Reconstruction
The goal of breast reconstruction is to restore a natural, realistic breast with adequate volume and shape and an aesthetically pleasing contour.
Being diagnosed with breast cancer begins a journey of making many informed decisions that deeply affect your body and mind. Using knowledge as a guide for your journey allows you to become an advocate for your own well-being. As a reconstructive plastic surgeon, Dr. Zemmel presents patients with the tools and information to build their knowledge as they embark on their journey. This page serves as an instrument of knowledge for past, current, and future breast cancer patients of Richmond Aesthetic Surgery as they make informed decisions about breast reconstruction. Remember, our surgeon will be there throughout this journey to guide, lead, or assist you with whatever you may need to succeed.
Reconstruction of a breast that has been removed due to cancer or other disease is one of the most rewarding surgical procedures our surgeon performs at Richmond Aesthetic Surgery. Recent advances in surgical techniques have made it possible for Dr. Zemmel to create a breast close in form and appearance to a natural breast. Frequently, reconstruction is possible immediately following breast removal (mastectomy), so patients awake from surgery with a reconstructed breast in place and are spared the experience of living without a breast. There are many options to consider as you and your surgeon explore what treatment course is best for you.
This information will give you a basic understanding of breast reconstruction — when it is possible, how and when it is performed, and what the journey entails. It will explain the pre-surgical plan, the surgical operation, and the post-surgical course, as well as the results you can expect. However, it cannot answer all of your questions since a lot depends on your individual circumstances. Please be sure to ask your surgeon if there is anything you do not understand about the procedures or what you can expect.
From the entire team at Richmond Aesthetic Surgery, we wish you the best of luck as well as good health and well-being during your journey.
Sincerely,
Neil J. Zemmel, MD, FACS*
I required bilateral mastectomies because of breast cancer. Dr. Z’s caring, guidance, and advice gave me results I never dreamed of! I am happier now with my body (at 55) than I was in my 30’s! I am SO glad I listened and took his advice. His concern and expertise are unmatched!
elizabeth chapman
June 11, 2012
Should I Get Breast Reconstruction?
Any patient who undergoes removal of a part of the breast (lumpectomy or breast conservation therapy), the whole breast (mastectomy), or preventive removal of the breast (prophylactic mastectomy) is eligible for breast reconstruction. New medical devices and plastic surgery techniques allow Dr. Zemmel to recreate a breast at the time of mastectomy or sometime later and to correct contour abnormalities of the breasts after breast conservation treatment. The best candidates, however, are women who are in good health, do not smoke, and whose cancer, as far as can be determined, will be or has been removed by surgery.
Many options are available for breast reconstruction. Your surgeon will recommend the best options for you based on your body size, shape, medical issues, personal values, personal preference, cancer, and need for chemotherapy or radiation. As you consider the options recommended by your surgeon at Richmond Aesthetic Surgery, ask yourself the following questions:
- How do I want to look in and out of my clothes?
- How much time am I willing to spend recovering from surgery?
- What physical activities do I participate in that could be affected by surgery to my belly, back, or buttocks?
Use the answers to these questions to help you choose which option you feel most comfortable with.
How Can I Prepare for Breast Reconstruction?
You can begin talking about reconstruction as soon as you are diagnosed with cancer, or when you find out that you are genetically predisposed to cancer. Our surgeon will work to develop a strategy to help put you in the best possible condition for reconstruction.
After evaluation, your surgeon will explain which reconstruction options are most appropriate for your age, health, anatomy, body type, and goals. Be sure to discuss your expectations openly. Post-mastectomy reconstruction can improve your appearance and renew your self-confidence — but keep in mind that the desired result is an improvement and not perfection.
Once you have scheduled a surgery date, your doctor will provide you with specific instructions on how to prepare for surgery, including guidelines on eating and drinking, smoking, and taking or avoiding certain medications or vitamins. Your doctor will also give you information regarding blood work and tests needed prior to surgery, and will have you receive a CT scan prior to any free-tissue breast reconstruction.
Immediate vs. Delayed Breast Reconstruction
Breast reconstruction can be done at the time of your mastectomy (immediate) or weeks, months, or even years later (delayed). The decision to have immediate or delayed reconstruction depends on many factors that Dr. Zemmel takes into consideration:
“When this happens to you, you do not want to wait weeks for questions. I was very pleased that I could get an appointment with Richmond Aesthetic Surgery within days.”
- Breast cancer stage
- Breast cancer tumor type
- Additional therapies (radiation or chemotherapy) to treat the cancer
- Other medical conditions (such as obesity, heart and lung conditions, and smoking)
- Your personal preference and lifestyle
Many choose to have delayed reconstruction based on these factors. Some women are not comfortable weighing all of their options during a time of extreme emotional stress when coping with the diagnosis of breast cancer. Some patients may be advised to wait because of other health conditions. Also, those with metastatic or inflammatory breast cancers may be advised to delay breast reconstruction. Your surgeon will discuss the advantages and disadvantages with you during your initial visit.
What Are My Breast Reconstruction Options After Mastectomy?
There are a number of ways to perform breast reconstruction after mastectomy. Dr. Zemmel divides them into three general categories:
- Breast reconstructions using prosthetic implants
- Breast reconstructions using your own tissue (autologous tissue reconstruction)
- Breast reconstruction using both implants and your own tissue
During your consultation, the pros and cons of each will be discussed with you, including the unique benefits and risks based on your situation. Your surgeon will also help you understand what to expect after your breast reconstruction process, which will likely require multiple surgeries. Together, you and your surgeon will choose the best option for you based on your body shape, past surgeries, current health, breast cancer treatments, and personal preferences.
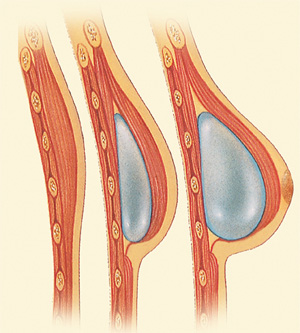
Breast Reconstruction with Implants
Breast implants can be used to restore the shape and volume of the natural breast tissue that is removed during cancer treatment, such as mastectomy. Our surgeon offers both saline and silicone breast implants for reconstruction, each coming in different shapes and sizes. Dr. Zemmel will go over the benefits and risks of your options, helping you determine which breast implant is ideal for your needs and preferences.
 If you choose to receive silicone breast implants, you will need to undergo an MRI every other year, starting three years after your reconstructive surgery, due to the risk of leaks going undetected. Saline implants, however, are more noticeable when there is a leak, which is why you will not need to undergo additional monitoring. Other complications associated with implants include infection, which occurs in less than 1% of cases at our practice, as well as capsular contracture, which is characterized by hardening of the scar tissue surrounding the implant. Capsular contracture happens in about 2-5% of cases and can constrict the breast implant, making it feel hard and look deformed. If you are undergoing radiation therapy, this increases your risk of capsular contracture, as radiation damages the surrounding tissues.
If you choose to receive silicone breast implants, you will need to undergo an MRI every other year, starting three years after your reconstructive surgery, due to the risk of leaks going undetected. Saline implants, however, are more noticeable when there is a leak, which is why you will not need to undergo additional monitoring. Other complications associated with implants include infection, which occurs in less than 1% of cases at our practice, as well as capsular contracture, which is characterized by hardening of the scar tissue surrounding the implant. Capsular contracture happens in about 2-5% of cases and can constrict the breast implant, making it feel hard and look deformed. If you are undergoing radiation therapy, this increases your risk of capsular contracture, as radiation damages the surrounding tissues.
Remember, implants are not lifetime devices and must be replaced like any other manufactured part. You should expect to replace your implants at least once in your lifetime. There is no mandatory scheduled maintenance, but the average patient replaces her implants around 10 to 15 years after surgery. A breast implant exchange procedure is usually simple with very little downtime. It requires no new incisions and is an outpatient operation.
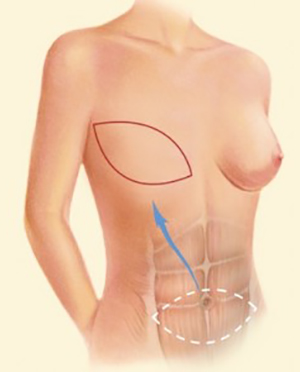
Breast Reconstruction with Your Own Tissue
Autologous tissue reconstruction, or flap reconstruction, involves using your own tissue from another part of your body to rebuild your breast. The tissue from your back, abdomen, thighs, or buttocks may be used. Sometimes, the tissue can stay connected to its own blood supply and just be rotated to reconstruct the breast, known as a pedicled flap. Other times, the tissue is disconnected from your body and its own blood supply and is reconnected to a new blood supply in the chest, known as a “free” flap. Free flaps typically do not require the sacrifice of a muscle in order to bring blood flow to the flap.
Regardless of which flap technique your surgeon performs, this type of reconstruction is more complex than implant-based reconstruction. Scars will be left at both the tissue donor site and reconstructed breast, and recovery will take longer than with an implant. On the other hand, when the reconstructed breast is made entirely with your own tissue, the results are more permanent, natural, and there are no concerns about implant-related complications. In some cases, you will have the added benefit of an improved body contour where the donor tissue was taken.
You will be required to stay in the hospital for 3 or 4 nights. During this stay, your surgeon and the nurses will monitor your flap to make sure the blood flow to the transplanted tissue is adequate. The color, temperature, and pulse of the skin will be checked. Two devices will be used to monitor your flaps. One listens to your blood flow through the flap (Doppler), while the other measures oxygen levels (ViOptix). If your flap has blood supply issues, your surgeon may have to take you back to the operating room to assess and correct the problem. This happens in less than 10% of patients. In approximately 2% of all patients, the flap may fail, and another method for your breast reconstruction will be offered.
You will also have 3 or 4 drain tubes placed depending on if one or both breasts are reconstructed. In most circumstances, these drains will remain in for about 10 to 14 days. The recovery time for flap reconstruction is approximately 4 weeks. You will likely be sore and bruised for 10 to 14 days. You should feel better each day, and our surgeon will make sure you are as comfortable as possible. You will have follow-up appointments with your surgeon at least once per week for the first month. It is very normal to feel fatigued in the few weeks following surgery.
What Are the Different Types of Flap Reconstruction?
The name of the flap for your autologous breast reconstruction denotes the area from which the tissue is taken (donor site). Common types of autologous reconstructions include:
- TRAM, DIEP, and SIEA Flaps: Tissue is harvested from the abdomen.
- T-DAP and Latissimus Dorsi Flaps: Tissue is harvested from the back.
- SGAP or LGAP Flaps: Tissue harvested from the buttocks.
- TUG Flap: Tissue is harvested from the thigh.
These surgeries require the skills of a microvascular-trained plastic surgeon. This is a complex technique that requires using a microscope to reconnect blood vessels. Dr. Zemmel offers these exciting new techniques.
Abdominal Wall Tissue (TRAM, DIEP, & SIEA Flaps)
An abdominal flap reconstruction may involve four layers of tissue taken from the abdomen:
- Skin and dermis
- Fatty tissue/subcutaneous tissue
- Thick connective tissue (fascia) that provides strength and structure to the abdominal wall
- Muscle layer where the rectus abdominis and obliques are located
The rectus abdominis muscle receives its blood supply from two blood vessels: the superior epigastric artery and vein, and the deep inferior epigastric artery and vein (DIEP). These vessels enter the body of the rectus muscle and branch within the muscle itself. The muscle then sends small blood vessels to the skin surface. Additional redundant vessels are located closer to the skin surface. These are called the superficial inferior epigastric artery and vein (SIEA).
Advances in surgical techniques have allowed surgeons to lessen the amount of muscle and fascia that is used for abdominal wall flaps. Now, Dr. Zemmel avoids taking any muscle or fascia by using the small blood vessels emanating from the muscle to the skin, called perforators. These perforators may come from the deep inferior epigastric vessels (DIEP) or from the more superficial source called the superficial inferior epigastric artery and vein (SIEA). Both the DIEP and SIEA are muscle sparing and use no muscle with the abdominal wall tissue, lowering the chance of hernia formation or abdominal wall bulge.
The amount of tissue and blood supply used to create your new breast determines the name of the breast flap. Your surgeon will help decide which type of flap is best for you.
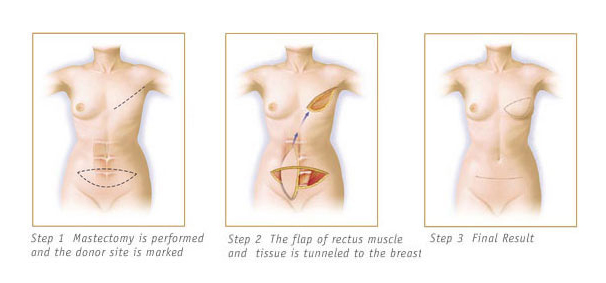
TRAM Flap
The TRAM (Transverse Rectus Abdominis) flap consists of skin, fatty tissue, and the rectus muscle itself. The TRAM flap is usually rotated on its remaining blood supply (pedicled) or disconnected from its own blood supply and reconnected to the blood in the chest (free flap). Since this flap involves removing your muscle, and sometimes your fascia, there is a small risk of hernia or weakness of the abdominal wall.
The pedicled TRAM flap operation is a safe, reliable procedure and has been offered for over 30 years. Your surgeon will examine you carefully to determine whether you are a candidate for a soft tissue reconstruction. They may offer you the options of either a pedicled TRAM flap or a DIEP or Free TRAM flap.
A free muscle-sparing TRAM flap is made up of belly skin, fat, and a very tiny part of the rectus muscle. This flap is disconnected from its own blood supply and then reconnected to the blood supply in the chest. If a large amount of muscle has to be taken because of the anatomy of your abdominal wall, then your surgeon may have to reinforce it with a supportive layer of mesh to prevent hernia formation.
DIEP Flap
A DIEP (Deep Inferior Epigastric Perforator) flap is made up of belly skin and fat ONLY. The flap is disconnected from its own blood supply and then reconnected to the blood supply in the chest using the deep inferior epigastric artery and vein and its perforators. This is the most common procedure performed by our Richmond plastic surgeon. Not only does the fat and skin removed at the time of surgery reconstruct a supple, naturally appearing breast, but it also provides for a “tummy tuck” effect.
There are a number of benefits of DIEP flaps over traditional pedicled TRAM flaps. They include:
- The ability to retain complete muscle function of the abdominal wall
- Reducing the risk of an abdominal wall hernia
- Elimination of prosthetic mesh placement in the abdomen
- Ability to shape a more natural, contoured breast
- Reducing the risk of fat necrosis
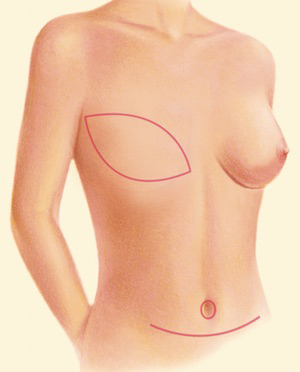
SIEA Flap
A free SIEA (Superficial Inferior Epigastric Artery) flap is made of belly skin and fat ONLY. The flap is disconnected from its own blood supply and then reconnected to the blood supply in the chest using the superficial inferior epigastric artery and vein and its perforators. Since the superficial epigastric artery and vein are very small, and only exist in about 30% of patients, few can have this flap.
Buttocks Tissue (SGAP & IGAP Flaps)
SGAP (Superior Gluteal Artery Perforator) and IGAP (Inferior Gluteal Artery Perforator) flap reconstruction is reserved for patients who do not have enough skin and tissue on the belly, have had previous belly surgery to preclude a DIEP, do not want implants, and have enough buttocks tissue to recreate a breast. These flaps are made of skin and fat from the buttocks. Their blood supply is disconnected from the buttocks and then reconnected to the internal mammary artery and vein in the chest. You will have a scar hidden in the bikini line and slight indent around the donor site area from where the tissue is taken. The SGAP and IGAP flaps provide for a natural-looking and moderate-volume breast.
Thigh Tissue (TUG Flap)
The TUG (Transverse Upper Gracilis) flap is made up of skin, fat and muscle from the thigh. The gracilis muscle that is taken is considered “expendable,” and patients do not report any weakness of the leg after surgery. The TUG is usually done for patients who do not have adequate skin in the buttocks or belly. It is a small-sized flap and thus can only be used for those who do not require a large-volume breast reconstruction. The incisions from the TUG are hidden in the groin area. This area is warm, moist, and dark, and it undergoes a lot of motion while sitting, standing, or using the bathroom which makes it a higher risk for poor healing and infection.
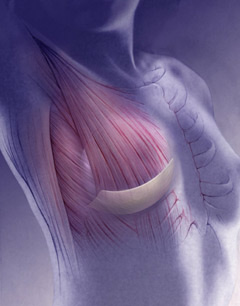
Back Tissue (Latissimus Dorsi & T-DAP Flaps)
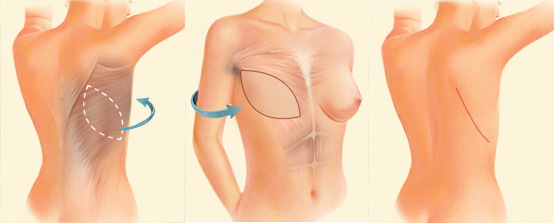
The latissimus dorsi flap from your back is made up of skin, fat, and muscle (latissimus dorsi muscle). The T-DAP (Thoracodorsal Artery Perforator) flap is made up from skin and fat ONLY. Both the latissimus dorsi and the T-DAP flaps remain attached to their blood supply and are rotated through the armpit to recreate the breast on the chest. The scar is often well-hidden in the bra strap on the back. Often, the flaps are not large enough to recreate a breast, and an implant will be required under the flap. People generally do not have a problem from missing the muscle in the back and continue their normal daily living. However, if you are a competitive rock climber, swimmer, or tennis player, you may be affected and show weakness.
How Long Does Breast Reconstruction Take?
The length of time for your breast reconstruction can vary depending on the number of surgeries you require and the need for other breast cancer treatments, such as radiation or chemotherapy. The reconstructive process generally takes 6 months to one year regardless of the type of reconstruction you choose, assuming no further cancer treatment is necessary. Some patients will require revisional surgeries to balance the reconstructed breast with the natural breast and recreate a nipple. The timeline to completion will vary for each patient, but a general guide is:
- Step 1: Mastectomy (with tissue expanders or a reconstruction immediately with a permanent implant or autologous tissue). Wait about 3 months for healing or 6-12 months if you need chemotherapy or radiation.
- Step 2: If you had tissue expanders at the time of your mastectomy, this will be when your surgeon recreates your breast (permanent implant or autologous tissue transfer). Wait 3 months for healing.
- Step 3: Surgery to make changes to the size and shape of your reconstructed or natural breasts as needed and perform nipple reconstruction. Wait 2-3 months for healing.
- Step 4: Nipple and areola tattooing in the office.
Single- vs. Two-Stage Breast Reconstruction
Within the implant-based reconstruction category, there are two possible methods of reconstructing the breast: two-stage reconstruction and single-stage reconstruction, also called direct-to-implant (DTI).
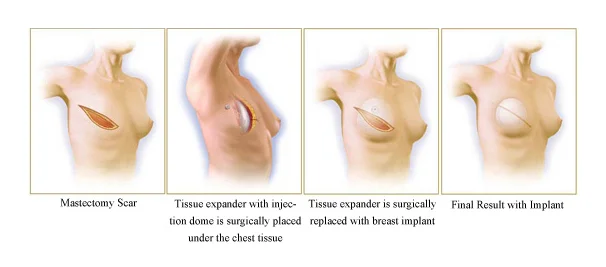
Two-Stage Breast Reconstruction
The first and most common technique, two-stage reconstruction, uses a device called a tissue expander followed by insertion of a prosthetic breast implant. This requires a minimum of two operations, and commonly a third is added to refine or “touch up” your result. Nipple reconstruction and fat grafting is usually performed at this third and final stage.
The first operation consists of mastectomy (removal of the breast, to be performed by the breast cancer surgeon) followed immediately by placement of a tissue expander with acellular dermal matrix (Alloderm). The purpose of the tissue expander is to stretch and mold the overlying soft tissue, skin, and muscle, and the goal of Alloderm is to create a stable pocket for your implant to permanently reside. This stretching and molding involves injections of a salt-water solution that typically begins immediately after surgery. The expander is inflated to approximately 50% to 75% of its final volume during the first procedure, and the remaining volume will be added during your follow-up visits over the course of 6 to 12 weeks after surgery.
Your surgery takes 1 to 1.5 hours for one side to be completed, longer if you are having surgery on both sides. You will be kept in the hospital overnight and should be able to go home in 1 to 2 days. This surgery will require placement of surgical drains to remove excess fluids from surgical sites immediately following the operation. In most circumstances, your surgeon will remove these drains when you come back for your 1 week or 2 week follow-up visit. If there is a lot of drainage, they will stay in for longer. You are likely to feel tired and sore for 1 to 2 weeks after reconstruction and take about 4 weeks to feel completely recovered. Most of your discomfort can be controlled by pain medication and muscle relaxants prescribed by our plastic surgeon.
The tissue expander process continues until the size is slightly larger than your desired reconstructed breast size. You may feel a sensation of stretching or pressure in the breast area during this procedure, but most women find it is not too uncomfortable. Filling of the expander stretches the skin and muscle to make room for a breast implant, much like a woman’s abdomen stretches during pregnancy. By filling the expander slowly over time, the tissue covering the implant is molded into a stable soft tissue pocket in preparation for the permanent implant insertion.
 After the skin over the breast area has stretched enough, the expander will be removed in a second outpatient operation, and a permanent implant will be inserted in its place. Oftentimes, “touch up” work is done to make the implant more symmetrical. Pocket work is performed along with autologous tissue fat transfer (fat grafting). The need of potential chemotherapy or radiation will affect the timing of your second-stage surgery. The second procedure typically is much less invasive and requires much less downtime compared to the first procedure. The nipple and areola (the dark skin surrounding the nipple) are usually reconstructed in a subsequent third procedure along with any final fat transfer.
After the skin over the breast area has stretched enough, the expander will be removed in a second outpatient operation, and a permanent implant will be inserted in its place. Oftentimes, “touch up” work is done to make the implant more symmetrical. Pocket work is performed along with autologous tissue fat transfer (fat grafting). The need of potential chemotherapy or radiation will affect the timing of your second-stage surgery. The second procedure typically is much less invasive and requires much less downtime compared to the first procedure. The nipple and areola (the dark skin surrounding the nipple) are usually reconstructed in a subsequent third procedure along with any final fat transfer.
The exchange of the tissue expander for a permanent implant takes about 1 hour for one side. Dr. Zemmel usually does not place surgical drains, and you can go home the same day as your surgery. You are likely to feel tired and sore for a week or so after the implant exchange. Much of your discomfort will be controlled by medication prescribed by our surgeon.
Dr. Zemmel performs the latest tissue expander reconstructions using acellular dermal matrix (Alloderm or Flex HD) techniques.
What Is Acellular Dermal Matrix (ACDM)?
ACDM is the dermal component of the skin donated for the purpose of reconstructive surgery. ACDM has been used for over 10 years in breast reconstruction and in other applications such as abdominal wall reconstruction. During breast reconstruction, ACDM is placed inside the breast where it can augment and reinforce your own tissues. In the setting of breast reconstruction, ACDM serves as a way to artificially and immediately lengthen the pectoralis muscle to create a breast pocket without the use of a tissue expander. It is an essential component for allowing single-stage breast reconstruction.
 ACDM is donated tissue that has been processed to remove all of the cellular materials leaving only the collagen scaffolding of the dermis. This means that the graft material has an extremely low rate of rejection. The graft has been tested for infectious diseases similarly to other donated tissues. Once ACDM is placed, your body will incorporate the graft into your own tissues. Over a period of 3 to 6 weeks, your own cells should repopulate the scaffolding, and your blood vessels will grow into it. The ACDM essentially becomes part of your body.
ACDM is donated tissue that has been processed to remove all of the cellular materials leaving only the collagen scaffolding of the dermis. This means that the graft material has an extremely low rate of rejection. The graft has been tested for infectious diseases similarly to other donated tissues. Once ACDM is placed, your body will incorporate the graft into your own tissues. Over a period of 3 to 6 weeks, your own cells should repopulate the scaffolding, and your blood vessels will grow into it. The ACDM essentially becomes part of your body.
The use of these artificial tissues has a number of advantages over traditional tissue expander techniques:
- Greater inflation during your initial operation
- Improved contour of the lower pole, or bottom of the breast
- Reinforces the soft tissue of the bottom of the breast for a more durable result
- May prevent scar tissue from forming around the final implant
- Stabilizes the crease (inframammary fold) of the breast
Single-Stage Breast Reconstruction
A single-stage direct-to-implant (DTI) breast reconstruction is completed in one surgical procedure at the same time as mastectomy. This eliminates the need for a tissue expander. Delayed reconstructions are typically not performed as the skin and overlying soft tissue become scarred and lose the elasticity needed to create a breast pocket. The breast cancer surgeon will normally perform a total nipple-areolar-skin sparing mastectomy. Your surgeon will then immediately begin the reconstructive procedure.
The skin flaps are examined to ensure good thickness and viability. The pectoralis major muscle is identified, and the muscle is raised from the chest wall. The serratus anterior muscle is also identified and raised in most patients to improve contour of the lateral mammary fold (side) of the breast. The acellular dermal matrix is then attached to the internal aspect of the inframammary fold, and the front edge of the serratus anterior muscle in a gentle arc to recreate the lower and side curves of the breast.
The upper border of the ACDM graft is then attached to the lower border of the pectoralis muscle to complete the breast pocket. The ACDM graft acts as a pectoralis major muscle extension. Multiple demo silicone implants are then placed in order to choose the optimal size and shape. A drain is then placed into the breast pocket to remove any fluid that may accumulate. Local anesthesia is injected into the pectoralis major muscle, serratus anterior muscle, and along the inframammary fold to give long-lasting pain relief after surgery. Finally, the upper and lower skin flaps are then redraped over the muscles and implants, and the incision is closed.
What Are the Benefits of Single-Stage Direct-to-Implant Breast Reconstruction?
There are a number of advantages to a direct to implant (DTI) reconstruction:
-
- Eliminates the need for two surgeries
- Avoids tissue expanders and the associated discomfort and recovery from the expansion process
- Requires only 1 drain per breast after surgery, and each drain is usually removed in half the time compared to tissue expander-based reconstruction
- A fully reconstructed breast is achieved after one operation, diminishing the patient’s overall stress — the improved psychological effects of this approach cannot be underestimated
Who Is a Candidate for Single-Stage Breast Reconstruction?
Many patients desiring single-stage DTI breast reconstruction seek out the care of Dr. Zemmel at Richmond Aesthetic Surgery. Their desire is to avoid multiple surgeries, shorten their recovery time, and avoid the tissue expander process. Optimal single-stage DTI reconstruction candidates have the following:
-
-
- Small breast cup sizes (typically sizes AA to C)
- Thick, healthy skin to cover the implants
- Normal BMI (body mass index)
- Will undergo total skin and nipple areolar sparing mastectomies
- Will not need radiation
- Little ptosis (sagging) of the breasts
-
Can Women with Large or Sagging Breasts Get Single-Stage Breast Reconstruction?
“When I came to the office, I was nervous because I did not know what to decide. The entire staff was there for me and I am so glad I chose Richmond Aesthetic Surgery for the reconstruction of my breast.”
Women who have larger breasts, or women whose nipples are low-set on the breast and face downwards, may not be optimal candidates for single-stage reconstruction. A number of more complex variables come into play. Each patient is unique and will be evaluated individually. Some important points to consider:
-
-
- Women who have larger breasts (D cup and larger) may require a large implant that cannot be placed at the time of initial mastectomy. In these women a tissue expander may be required to stretch the overlying muscle to accommodate the larger implant size.
- Larger-breasted women may require removal of breast skin. Adding these extra incisions can further alter the blood flow to the skin flaps making the flaps less reliable. In this case placing a tissue expander is necessary.
- In women with larger breasts who undergo nipple-sparing mastectomy for cancer treatment, the nipple may be in too low of a position for a single-stage reconstruction, and a tissue expander may be required.
- In women undergoing prophylactic mastectomy (preventative mastectomy for BRCA+ patients) who have larger breasts, a preemptive breast reduction or mastopexy (lift) can be performed. This reduces the breast volume and places the nipple and areola in the optimal position for a single-stage mastectomy and reconstruction. The mastectomy and reconstruction is performed 6 to 12 months after the preemptive first procedure.
-
What Is Recovery Like After Single-Stage Breast Reconstruction?
Recovery from total skin-sparing mastectomy with immediate single-stage reconstruction typically takes between 10 and 14 days. Most of the recovery stems from the stretching of the pectoralis major muscle overlying the implant. Despite placement of ACDM to extend the muscle, the muscle still must accommodate the implant. Most women will state that they have severe muscle soreness, which typically begins to resolve around 7 days after surgery. The incisions themselves are usually numb from the mastectomy. During surgery, Dr. Zemmel will inject a new anesthetic medicine into your muscles and along the suture line of the ACDM graft. This new medicine is a long-lasting local anesthetic (liposomal bupivacaine) designed to last 3 days. This will reduce your pain level by approximately 50%.
Your surgeon will ask you to refrain from heavy lifting and raising your arms above your head for about 7 days. This allows your incisions to heal and the muscle to rest while accommodating the implant. After one week you will be encouraged to use your upper extremities for light activities of daily living. After 2 to 3 weeks, your surgeon will prescribe physical therapy to loosen your pectoralis muscles and to increase shoulder strength.
Initially, you will have some mild to moderate swelling and bruising around the breasts. This will take between 2 and 3 weeks to resolve. You may notice the implants in a slightly higher position on the chest wall. Your implants will descend into their final position during the first 4 to 6 weeks. Your breasts should also soften during this time and feel more comfortable.
When Will I Need to Return for Follow-Up Appointments?
Your first follow-up visit after your breast reconstruction will be within the first 5-7 days after you are discharged from the hospital. At this visit, your plastic surgeon will see how your newly reconstructed breasts are healing, as well as your donor sites. You may have one or more of your drains pulled if they are ready; sutures may also be removed; and a thorough examination will assure that you are on the proper post-operative track. Your surgeon will discuss the next step in the process and answer any questions you may have regarding activity or anything else.
Nipple & Areola Reconstruction
Once you and your surgeon are pleased with the shape, size, and symmetry of your breast reconstruction, and you have had time to heal, you may consider having nipple reconstruction.Your reconstructed nipple will be different than a natural nipple. It will not have temperature or other sensation and may have a different texture. Your nipple will be for cosmetic purposes and not be functional. Dr. Zemmel believes that nipple-areola reconstruction completes your reconstruction, adding the “finishing touches.” Please note that all insurance companies cover nipple-areola reconstruction as part of breast reconstruction.
If you choose to have your nipple reconstructed, there are different options.
-
-
- Tattoo Only: First, you can choose to have a 3-D tattoo only without surgery. This gives the appearance of a nipple and areolar but does not actually have a protruding nipple.
- Tattoo with Added Skin Bump: A second option, and most common, is to use the skin of your reconstructed breast to recreate a nipple. This is a small outpatient procedure with little recovery time. This nipple bump will be the color of your reconstructed breast skin, and will not have an areola (colored portion around the nipple). The areola and nipple can then be colored using a tattoo. The tattooing can be done at Richmond Aesthetic Surgery.
- No Nipple Reconstruction: The third option is not to have a nipple reconstructed at all. Our plastic surgeon will guide you through this decision-making process and help you reach the best decision.
-

What Risks Are Associated with Breast Reconstruction?
Dr. Zemmel will do everything possible to minimize the complication rate of your surgery. Despite best efforts, however, certain complications can occur. They can range from mild asymmetry to significant skin and tissue necrosis. The standard surgical complications include bleeding, infection, damage to surrounding tissue structures, pulmonary embolism, deep venous thrombosis, skin flap necrosis, capsular contracture, implant rupture, and major asymmetry. Your surgeon will go over the rates of these complications during your consultations.
The procedures recommended by our surgeon are relatively safe and low risk. He will discuss the risks, benefits, and alternatives to each procedure at length during your pre-operative consultations. Their primary goal is to provide you with a safe, reliable procedure while minimizing your risks. However, there are certain aspects of your healing that your surgeon will have no control over.
The predictability of healing will depend on your skin, underlying muscle and bony structure, genetic influences, and lifestyle factors such as diet, exercise, and smoking. Remember: you will be a work in progress for 6 months to one year. Your final result will take time to evolve and mature. Slight irregularities and undercorrection or small scars may result. Minor revisions after surgery are preferable to excessive operation and over-operation at the initial procedure.
Plastic surgery is a combination of art and science, and it is not an exact science. Some of the factors involved in the outcome (such as your specific healing characteristics) are not within your surgeon’s control, and therefore, it is not possible to guarantee a result. Dr. Zemmel guarantees his credentials, best effort, honest education, training, and compassionate care individualized to your needs. He is invested in your care and your outcomes; he will treat you like family.
What Can I Expect in My Breast Reconstruction Recovery?
Many women want to know when they can get back to doing everyday things like driving, exercising, and returning to work. This will vary depending upon the type of surgery you have had and upon you as an individual. Every woman will heal at her own pace, and getting back to “normal” is a process.
It is usually fine to start driving again when you feel that you could safely do an emergency stop or move the steering wheel around suddenly and are NOT taking any pain medicine. Some women find this possible to do within 10 to 14 days after surgery, and others find it takes longer.
Follow your doctor’s advice on when to begin stretching exercises and normal activities. As a general rule, you will want to refrain from any overhead lifting, strenuous sports, and sexual activity for 2 to 4 weeks following reconstruction. You will also be referred to a physical therapist after your surgery for exercises to help with recovery.
Reconstruction cannot restore normal sensation to your breast, but in time, some feeling may return. Never place a heating pad or ice pack on your breast after you have had a mastectomy for the risk of possible burns or frostbite. Ask our surgeon about the possibility of undergoing the highly innovative technique of reconnecting nerves during DIEP flap surgery.
Is Breast Reconstruction Covered By Insurance?
The 1998 Women’s Health Care and Cancer Rights Act (WHCRA) guarantees coverage for breast cancer treatment and breast reconstruction. It protects the rights of women who undergo mastectomy and desire reconstruction. The surgeries that must be covered include:
-
-
- Partial or total mastectomy (removal of the breast) due to cancer
- Reconstruction of the breast that was partially or totally removed by mastectomy
- Surgery and reconstruction of the natural, unaffected breast to make the breasts look symmetrical or balanced after mastectomy
- External breast prostheses that fit into your bra that are needed before or during the reconstruction
- Any downstream maintenance required for implant-based reconstruction
- Nipple and areolar reconstruction
-
Your insurance carrier is federally mandated to cover these procedures. Your normal co-pays, deductibles, and out-of-pocket maximums will apply. If you have questions regarding insurance coverage, please speak with the billing manager at Richmond Aesthetic Surgery or your plastic surgeon.
Additional Frequently Asked Questions
How Will Radiation Affect My Breast Reconstruction?
Radiation affects every patient differently but can cause hyperpigmentation (skin color changes like a sunburn) and changes in the texture and quality of the skin, muscle, and tissues inside the breast pocket after mastectomy. This firmness of the tissues is known as radiation fibrosis. To prevent this radiation fibrosis from damaging the breast reconstruction, your surgeon may recommend having a staged surgery, using a tissue expander beneath the breast at the time of mastectomy, especially if you are planning on having autologous tissue for reconstruction.
Your surgeon may recommend having a tissue expander if you are having radiation therapy because there are increased risks for complications while undergoing radiation therapy. If you are having an autologous breast reconstruction, your surgeon alternatively may choose to perform your reconstruction at the time of your mastectomy but make the breast larger in volume to allow for the radiation fibrosis changes to the reconstructed breast. If your surgeon recommends having a tissue expander, you may undergo radiation treatment with the tissue expander in place. Then later, your surgeon will replace the expander and reconstruct your breast with autologous tissue or an implant of your choice.
Studies have shown that patients who have radiation therapy are at an increased risk for problems with permanent implants. These problems include capsular contracture (scarring and distortion of the breast), infection, and wound healing problems necessitating the removal of the implant. Dr. Zemmel will help you to make an informed decision if you are to undergo radiation therapy.
Can You Have Breast Reconstruction During Chemotherapy?
Breast reconstruction should not delay chemotherapy. Your medical oncologist will begin chemotherapy once your incisions are fully healed and your drains have been removed. If you have a tissue expander placed at the time of your mastectomy, you may have your chemotherapy while undergoing tissue expansion. Tissue expansion may continue as long as you are comfortable, have no infections, and your blood counts are stable. Dr. Zemmel prefers to fill your expanders about 2 days before your chemotherapy dose, as this is when your blood counts are highest.
Does Breast Reconstruction Increase the Risk of Cancer Returning?
NO. The risk of breast cancer returning (recurrence) depends on the stage of the breast cancer, the type of breast cancer (hormone receptors), and additional therapies (chemotherapy or radiation) used to treat breast cancer. Reconstruction has no known effect on the recurrence of cancer in the breast, nor does it interfere with detecting cancer if it does in fact return.
The surgical, medical, and radiation oncologist will discuss your risk of cancer recurrence with you and decide upon the methods or tests used to detect the cancer. Dr. Zemmel may recommend continuation of clinical breast exams on the reconstructed breast. If your breast reconstruction involves a silicone implant, the FDA recommends that you get an MRI to check for rupture 3 years after surgery, and then every 2 years thereafter.
<h3″>Will My Breast Reconstruction Results Look Natural?
Dr. Zemmel will make every effort to create a natural, proportional breast. Reconstructed breasts, however, will be different from the natural breasts with which you were born. Your reconstructed breast may feel slightly firmer and may have a somewhat different shape than your natural breasts. It may not have the exact same contour as your breast and before mastectomy.
In the case of a unilateral (one-sided) breast reconstruction, your reconstructed breast may not exactly match your opposite breast. Therefore, a symmetry matching procedure may be necessary to obtain optimal symmetry. However, these small revision surgeries (“touch ups”) may improve contour and symmetry. These differences will generally be apparent only to you. Therefore, you should decide what differences you would like to change and discuss them with your surgeon.
For most mastectomy patients, breast reconstruction dramatically improves their appearance and quality of life following lumpectomy or mastectomy surgery.
Will I Need My Breast Reconstruction Revised Later?
At Richmond Aesthetic Surgery, most patients who undergo breast reconstruction with a single-stage direct-to-implant reconstruction do not require major revision. It is not uncommon, however, to need “touch ups.” Touch ups can be considered minor procedures to improve the appearance of the breasts and may include:
- Scar and dog ear revisions
- Autologous tissue fat transfer (fat grafting) for contour improvement
- Implant exchange for volume asymmetries
Most breast reconstruction involves a series of procedures that occur over time. Usually, the initial reconstructive operation is the most complex. Follow-up surgery, or revisions, may be required to enlarge (breast augmentation), reduce, or lift (mastopexy) the natural breast to match the reconstructed breast. It is almost always performed to improve the symmetry, shape, size, and/or contour of the reconstructed breast itself.
Often, improvements in the contour and symmetry of the reconstructed breast are accomplished by using fat grafting. In this procedure, fat is taken by liposuction from an area of the body (belly, thighs, or buttocks) and then injected into the reconstructed breast where symmetry and contour is needed. These secondary procedures are outpatient procedures and rarely require the use of drains. The recovery time is based on the extent and complexity of the procedure, but usually ranges from 5 to 10 days.
Schedule Your Breast Reconstruction Consultation
Dr. Zemmel would like to thank you for choosing Richmond Aesthetic Surgery to provide your care, and he looks forward to helping you on your journey. We wish you all of the best.
To learn more about breast reconstruction options, or to schedule a consultation with our experienced plastic and reconstructive surgeon, please contact Richmond Aesthetic Surgery.